CPC AAPC Certified Professional Coder (CPC) Exam Free Practice Exam Questions (2025 Updated)
Prepare effectively for your AAPC CPC Certified Professional Coder (CPC) Exam certification with our extensive collection of free, high-quality practice questions. Each question is designed to mirror the actual exam format and objectives, complete with comprehensive answers and detailed explanations. Our materials are regularly updated for 2025, ensuring you have the most current resources to build confidence and succeed on your first attempt.
A physician prescribes carbamazepine to treat a patient with epileptic seizures. After six months, the physician performs a therapeutic drug test to monitor the total level of the drug in the patient.
What CPT® and ICD-10-CM coding is used for the six month-evaluation?
A 55-year-old patient with suspected liver cancer was seen by the physician to obtain a biopsy. The special biopsy needle was placed using ultrasonic guidance. The physician obtained a small tissue sample from the liver, which was then sent to pathology.
What CPT® codes are reported?
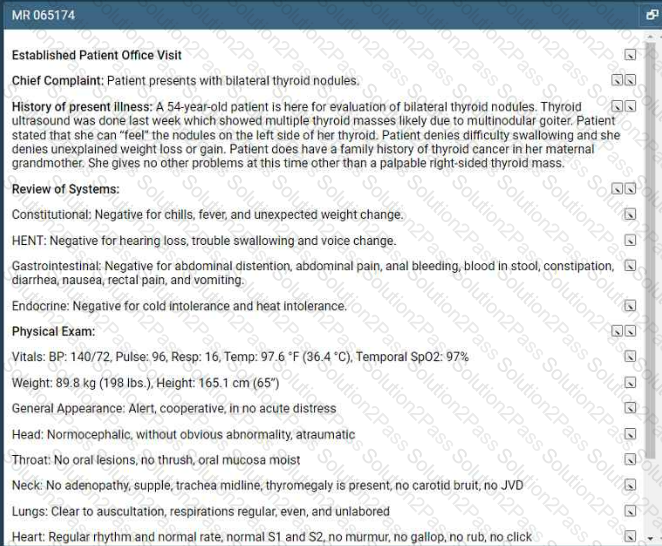
Refer to the supplemental information when answering this question:
View MR 065174
What E/M code is reported for this encounter?
A patient's left eye is damaged beyond repair due to a work injury. The provider fabricates a prosthesis from silicon materials and makes modifications to restore the patient's cosmetic appearance.
What CPT® code is reported?
View MR 001394
MR 001394
Operative Report
Procedure: Excision of 11 cm back lesion with rotation flap repair.
Preoperative Diagnosis: Basal cell carcinoma
Postoperative Diagnosis: Same
Anesthesia: 1% Xylocaine solution with epinephrine warmed and buffered and injected slowly through a 30-gauge needle for the patient's comfort.
Location: Back
Size of Excision: 11 cm
Estimated Blood Loss: Minimal
Complications: None
Specimen: Sent to the lab in saline for frozen section margin control.
Procedure: The patient was taken to our surgical suite, placed in a comfortable position, prepped and draped, and locally anesthetized in the usual sterile fashion. A #15 scalpel blade was used to excise the basal cell carcinoma plus a margin of normal skin in a circular fashion in the natural relaxed skin tension lines as much as possible The lesion was removed full thickness including epidermis, dermis, and partial thickness subcutaneous tissues. The wound was then spot electro desiccated for hemorrhage control. The specimen was sent to the lab on saline for frozen section.
Rotation flap repair of defect created by foil thickness frozen section excision of basal cell carcinoma of the back. We were able to devise a 12 sq cm flap and advance it using rotation flap closure technique. This will prevent infection, dehiscence, and help reconstruct the area to approximate the situation as it was prior to surgical excision diminishing the risk of significant pain and distortion of the anatomy in the area. This was advanced medially to close the defect with 5 0 Vicryl and 6-0 Prolene stitches.
What CPT® coding is reported for this case?
This 27-year-old male has morbid obesity with a BMI of 45 due to a high calorie diet. He has decided to have an open Roux-en-Y gastric bypass. The patient is brought to the operating room and placed in supine position. A midline abdominal incision is made. The stomach is mobilized, and the proximal stomach is divided and stapled creating a small proximal pouch in continuity with the esophagus. A short limb of the proximal bowel of 155 cm is divided. It is brought up and anastomosed to the gastric pouch. The other end of the divided bowel is connected back into the distal small bowel to the short limb's gastric anastomosis to restore intestinal continuity. The abdominal incision is closed.
What are the procedure and diagnosis codes for this encounter?
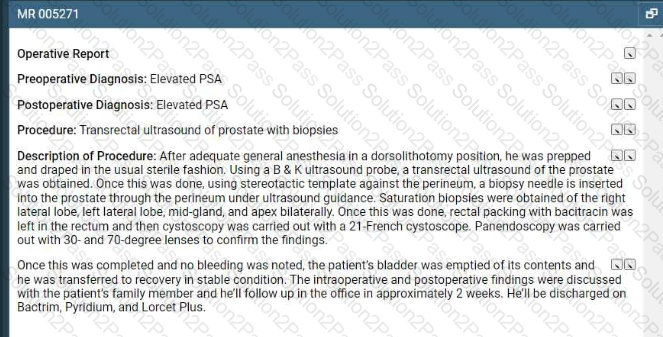
Refer to the supplemental information when answering this question:
View MR 005271
What CPT® coding is reported?
A patient in a radiology facility has an X-ray examination of her lumbosacral spine due to pain while playing golf. The radiologist takes a complete 7-view of the lumbosacral spine, including
bending views.
What CPT® code is reported?
The provider orders a bile test for a patient that has chronic hepatitis that is undergoing treatment. Lab analyst quantitates the total bile acids with an enzymatic method. What CPT® code is
reported for the test?
Mrs. Wilder presents with right and left leg swelling. Venous thrombosis imaging of each leg is done and shows deep venous embolism and thrombosis in each leg.
What CPT® and ICD-10-CM codes are reported?
View MR 003396
MR 003396
Operative Report
Preoperative Diagnosis: Acute MI, severe left main arteriosclerotic coronary artery disease
Postoperative Diagnosis: Acute MI, severe left main arteriosclerotic coronary artery disease
Procedure Performed: Placement of an intra-aortic balloon pump (IABP) right common femoral artery
Description of Procedure: Patient's right groin was prepped and draped in the usual sterile fashion. Right common femoral artery is found, and an incision is made over the artery exposing it. The artery is opened transversely, and the tip of the balloon catheter was placed in the right common femoral artery. The balloon pump had good waveform. The balloon pump catheter is secured to his skin after local anesthesia of 2 cc of 1% Xylocaine is used to numb the area. The balloon pump is secured with a 0-silk suture. The patient has sterile dressing placed. The patient tolerated the procedure. There were no complications.
What CPT® coding is reported for this case?
A patient suffers a ruptured infrarenal abdominal aortic aneurysm requiring emergent endovascular repair. An aorto-aortic tube endograft is positioned in the aorta and a balloon dilation is performed at the proximal and distal seal zones of the endograft. The balloon angioplasty is performed for endoleak treatment.
What CPT® code does the vascular surgeon use to report the procedure?
A surgeon performs a complete bilateral mastectomy with insertion of breast prosthesis at the same surgical session.
What CPT@ coding is reported?
A patient complains of tarry, black stool, and epigastric tightness. An esophagogastroduodenoscopy is recommended to evaluate the source of the bleeding. The endoscope is inserted orally. The esophagus appears normal on scope insertion. No evidence of bleeding in the stomach. The scope is then passed into the duodenum, where a polyp is found and removed with hot biopsy forceps. No evidence of bleeding post procedure.
What CPT® code is reported?
Dr. Burns sees newborn baby James at the birthing center on the same day after the cesarean delivery. Dr. Burns examined baby James, the maternal and newborn history, ordered appropriate blood test tests and hearing screening. He met with the family at the end of the exam.
How would Dr. Bums report his services?
Ms. C is diagnosed with a supratentorial intracerebral hematoma, and the neurologist performs a craniectomy to access the hematoma. The hematoma is accessed, and a suction device is
used to remove it.
What CPT@ code is reported?
A patient with Parkinson's has sialorrhea. The physician administers an injection of atropine bilaterally into a total of four submandibular salivary glands.
What CPT® coding is reported?
Which place of service code is submitted on the claim for a service that is performed in an outpatient surgical floor?
